Have you put off doing the dental work you need because you are afraid it might fail? You may have had the right idea! Have you heard that all root canals are bad for you? Or that a titanium implant blocks the meridian flow, or can corrode because of the acids in your mouth? Or that extractions are bad for you because they might lead to cavitations or dry sockets? In fact, all the above are possible. If you are immune compromised in any way, pay attention, because what you are going to learn here can make a difference between success and failure when it comes to dental surgery of any kind, whether it be root canals, implants, extractions or even gum procedures like deep cleanings.
How systemic inflammation can affect dental health
Inflammation is similar to stress in that short-term stress is considered fine and doesn’t affect our health. The fight or flight response has kept us alive when threatened with danger. However, long-term stress is a totally different situation and has been identified as a co-factor in most serious health conditions. Similarly, short-term inflammation is actually vital in our ability to heal from injury, toxicity, and infection, however, long-term inflammation can make us ill because it leads to the breakdown of our immune system and organs. In short, chronic inflammation negatively affects our ability to heal.
I think most people and M.D.’s would agree that inflammation is not healthy when extended over a long period of time. There is an inflammatory component to almost every chronic disease including strokes, heart disease, all autoimmune diseases, cancer, arthritis, etc. That’s why some doctors call inflammation ‘The Silent Killer.’
So how does chronic inflammation affect our oral health and ability to heal from dental surgery? Actually, more than we have thought in the past. Traditionally, dentistry has been thought to be somewhat a sub-specialty within medicine but recent research has begun to make connections between dental health and overall health. For instance, there is ample research linking gum disease to heart disease, strokes, arthritis, and diabetes. However, until fairly recently, there has not been a lot of research linking root canal infections with systemic diseases like heart disease.
In an article published in February 2014 in JOE, which is the Journal of Endodontics, the researchers found that the patients with infected root canals had 2.79 times higher risk of developing coronary artery disease. (1)
The best way for me to put this into perspective is to give you an example. Recently a patient came to me to find out what her options were after an implant had failed and had been removed by the dentist that placed it. When she relayed her experience, she told me that there was a lot of pain and infection caused by the implant almost immediately after placement. What caused this pain and swelling and what caused the implant to fail? The rest of this article is dedicated to a little-known fact that results in failures of implants, root canals, deep cleanings and gum surgery.
Case Study
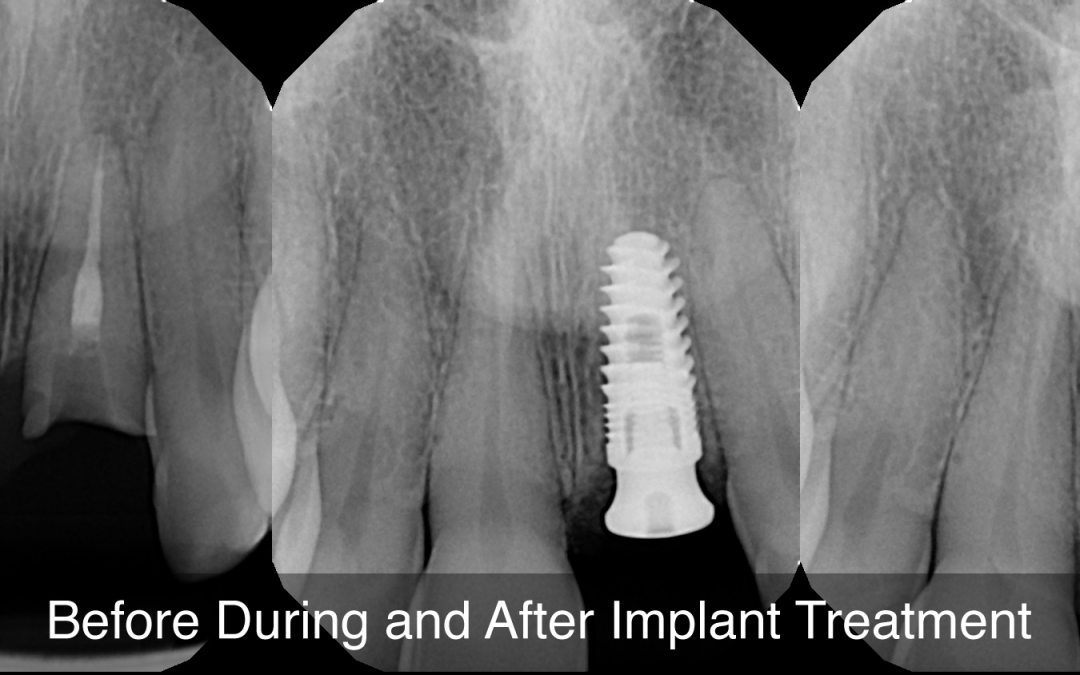
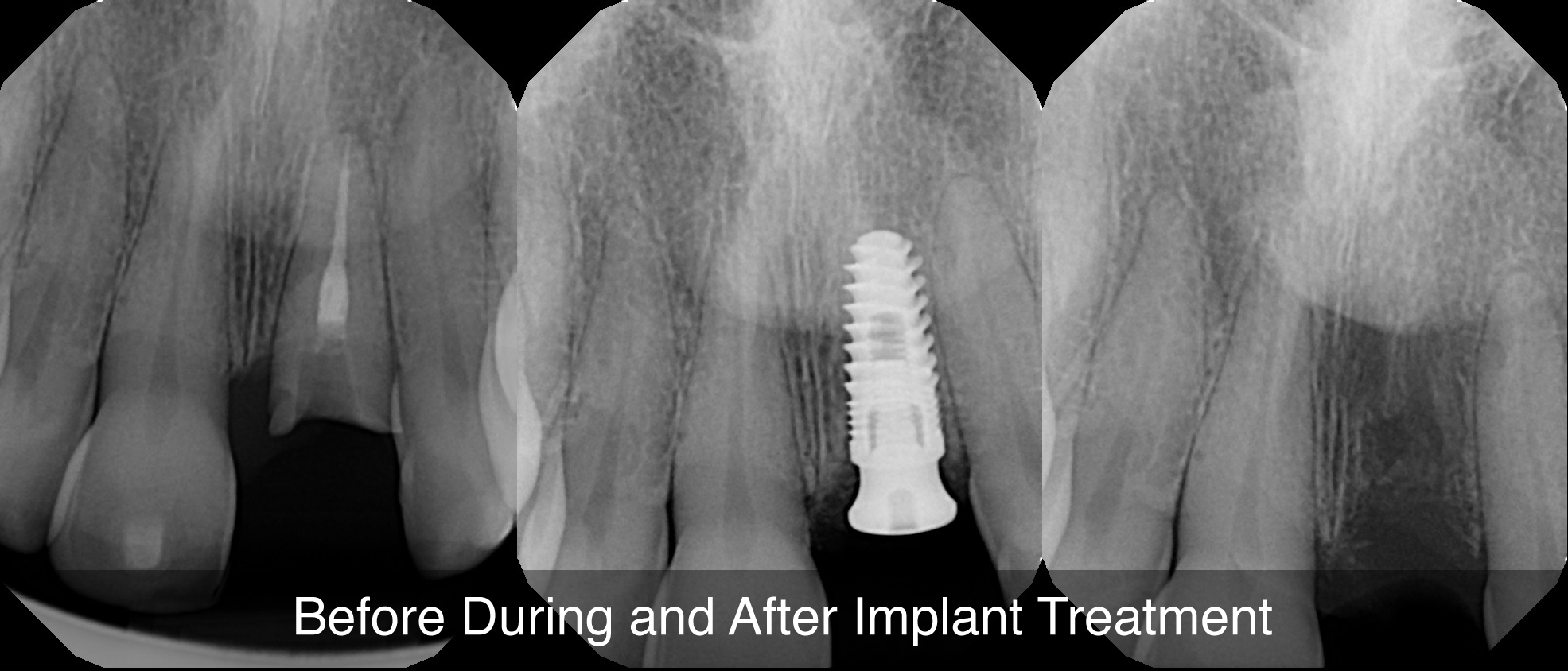
Here is a brief history of a patient’s experience with an infected and broken tooth and a subsequent implant placed to replace tooth #9, which is the front tooth on the left side.
When this patient presented to me, she reported the following health problems and medical conditions:
- Fibromyalgia post car accident 1992.
- Irritable Bowel Syndrome – IBS
- Food intolerance gluten, dairy (family history)
- Shrimp allergy- severe anaphylactic. Can eat all other shellfish, which I find weird
- Allergic reactions to Bactrim (rash) and Mucinex (bleeding)
- Itching reaction typical when taking meds like Ultram, Percocet.
- Pre-diabetic in late 2016, but next labs in 2017 HbAIc was normal (diabetes in
family ) - History of high blood pressure, worse since implant.
- History of high cholesterol
- Osteoarthritis in knees, hips, low back, neck
- Overweight by about 30 lbs
Every single one of the things she reported above indicates inflammation. and this could be affecting her ability to heal. Here is a summary of the patient’s experience:
- August 2016, my tooth cracked in two places: by the root and in the middle.
- I then consulted 6 different dentists, 1 oral surgeon, 3 general dentists, 1 periodontist and 1 prosthodontist, all of whom said it could not be fixed and an implant was recommended.
- In Sept 2017, I learned of a general dentist who did implants and accepted Medicare, which would pay for some of the costs, about 3k.
- On Jan 3, 2018, I had the first bone graph to start the implant process. The bone graft was intense and more painful afterward than I expected. I was not given an antibiotic.
- At the end of April, I had a 3D scan taken. I was told all looked fine to continue with the implant on May 1, 2018.
- May 1, the implant was placed and it was highly traumatic during and after. I was in intense pain and swelling on my left side of the face, including my nose, lips, and cheek for about the first 6 days.
- The doctor was going to prescribe amoxicillin for 10 days, but I told him I cannot tolerate that antibiotic as I get severe diarrhea (I already have IBS).
- He also told me to take Ibuprofen and I told him that I get rectal bleeding. He said to take Tylenol then. A lot of pain persisted to the point I was crying.
- Unbeknownst to me, I had an infection. I called the doctor less than 2 days after the implant and told him my pain was so intense that I wanted some Percocet. He told me to try Tylenol, and if it didn’t work to call him the next day, which was a Friday.
- I was so mad that I didn’t call him the next day to tell him I still needed the Percocet.
- I had a follow up 1 week later and told him of my horrible pain and swelling and emotional trauma, and that he should have prescribed the Percocet. He listened but still said he felt I tied his hands.
- Fifteen days later, May 16, the implant became loose and started dropping. I went to the dentist for an ER visit to remove the implant. That was incredibly traumatic and painful. He said I had an infection which ate some of the bone, that my body rejected the implant and we were going to have to let it heal for about a month and start all over with a 2nd bone graft.
- My bp was normal that morning, but I could tell it might be high because of the amount of stress I felt during the removal. It was 193/113. NEVER in my life had bp over 158/100, which is high enough! This time he gave me Percocet. I took 2 doses.
- I had a follow up to check tissue healing 2 weeks after removal and he said I have a divot, where my tissue makes a sort of hole inside where the implant would go.
- What I have experienced in pain and trauma, as well as the time I’ve lost in getting the final crown, I can’t get back. I should have been completely done April or May of this year.
Take a blood test before dental work
When this patient first requested an appointment, after reviewing the above history, I immediately requested that she take a blood panel. It is my opinion that when a patient has a compromised immune system or has chronic systemic inflammation, it’s important to look at blood work. When dealing with systemic issues like diabetes and autoimmune disease, I always recommend blood testing before any involved dental treatment. The reason for this is that certain inflammatory markers in the blood can signal a possible problem during the healing phase after procedures like extractions, implants and sometimes even root canals. The last thing you or I want is for there to be a failure in treatment requiring you to undo all the hard work you have put into your teeth.
The markers I look at as indicators of systemic inflammation:
- Vitamin D levels
- Immune cell levels
- Fibrinogen, homocysteine and especially CRP
- Blood sugar and HbA1c levels (a marker for glucose) which most people don’t realize can affect your ability to heal
- Hormone levels and autoimmune markers, especially for the thyroid gland
- Triglycerides ( a marker associated with heart disease)
- LDL levels and LDL/HDL ratio associated with cholesterol
What the blood test showed
Marker Normal Range Patient Level
Vitamin D 30-100 25.7 low
Glucose 65-99 100 high
HbA1c 4.8-5.6 5.8 high
Triglycerides 0-149 300 high
LDL 0-99 158 high
Cholesterol 100-199 267 high
As you can see from the above chart, this patient is high in inflammatory blood markers, indicating that she has a high level of systemic inflammation, which is a warning sign before doing any major dental work.
Supplementation
Why vitamin D is vital to dental health
Why did I put Vitamin D at the top of the list? Vitamin D, as we are finding out, is critical for modulating other hormones, bone health, healing from any surgery involving bone, modulating inflammation in the body and our normal immune function. Vitamin D mediates CA absorption and mineral homeostasis. It is also critical for bone growth hormones and plays a role in reducing the effects of inflammation.
This is why I recommend Vitamin D to any patient who is trying to lower inflammation or facing any significant dental treatment or surgery. I wrote an article on nutrition, blood markers and dental health that is on my homepage. If you want to read it go over to this page. Many of the markers and nutrients listed above are discussed there in more detail.
Dr. O’s recommendations
The premise of this article is that inflammation affects dental health and the outcome of major dental procedures. I believe it’s best to address systemic inflammation before it leads to failures in your dental treatment.
With the patient above, before any more dental work was done, I recommended nutritional counseling and supplementation with Vitamin D, high-quality fish oil, Vitamin C and some tissue-specific products for bone and soft tissue health. For more information as to what may be applicable in your case, you may call our office and set up a consultation with me, Dr. ORielly. Or, you can call for a nutritional and dental assessment with Victoria who is Dr. O’s wife and a nutritionist.
To read more about what Dr. O recommends for root canals, click here:
To learn about what Dr. O recommends for implants, go to:
References:
- Association between Chronic Apical Periodontitis and Coronary Artery Disease, JOE, February 2014 Volume 40, Issue 2, Pages 164–167; Tatiana Hassin Rodrigues Costa, MSc, José Albuquerque de Figueiredo Neto, PhD, Ana Emilia Figueiredo de Oliveira, PhD, Mariana de Figueiredo Lopes e Maia, MSc, Aiza Leal de Almeida, MSc
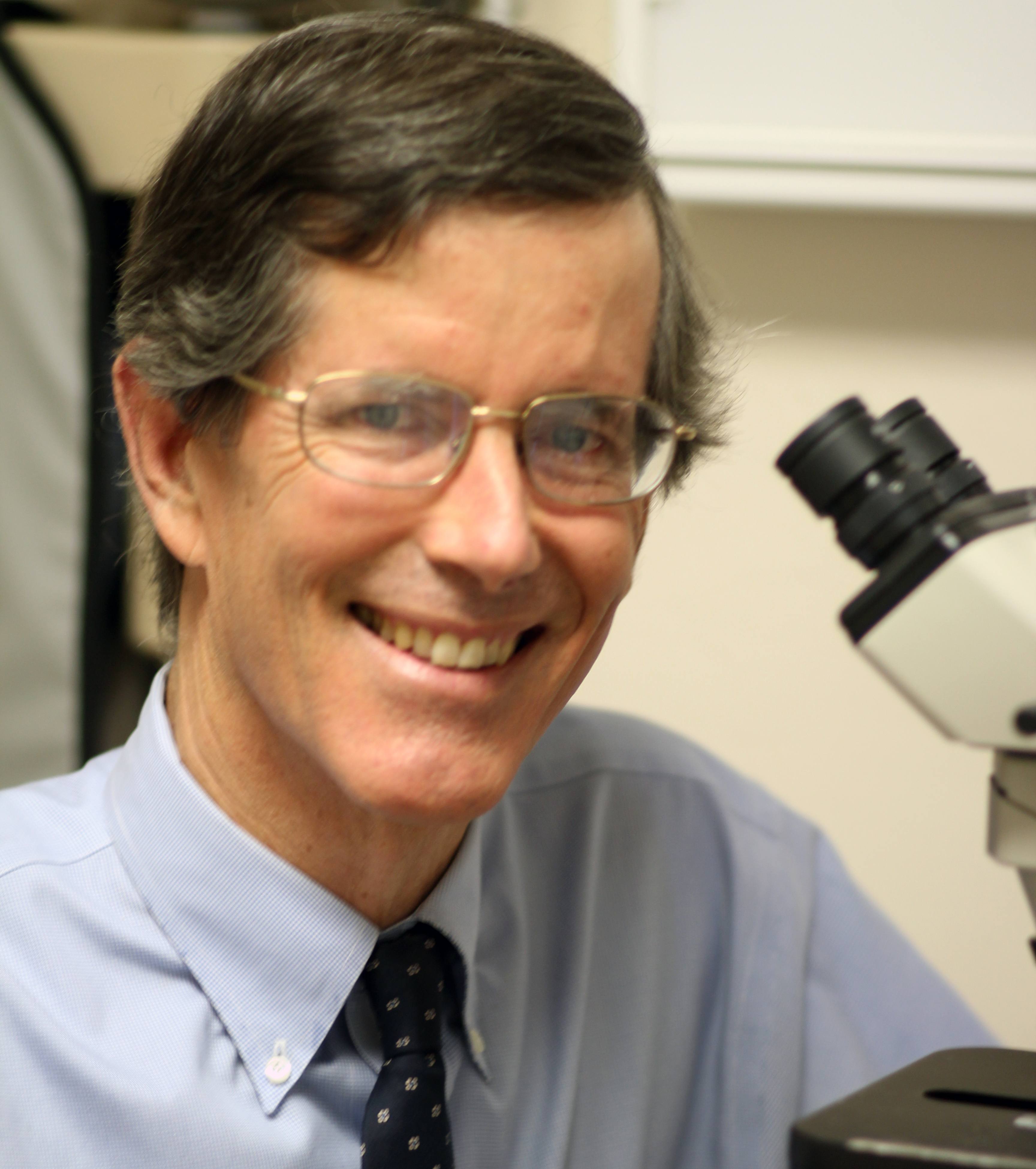
Carey O’Rielly DDS has been a practicing dentist for 35 years. He went to USC Dental School and Duke University for his undergraduate degree. He grew up in Laguna Beach and now lives in La Costa with his wife Victoria, who runs his office.
He began his career by owning and operating a network of six offices in the San Francisco Bay Area. Presently he owns a private holistic practice in North County San Diego’s Encinitas.
Dr. O started looking for solutions to his health challenges that resulted from the stress and environmental toxicity that built up over a ten year period running his dental network. He has dedicated himself to learning about oral systemic problems and how dentistry can affect your health. He has applied what he has learned over the last twenty years to ensure he, his staff and his patients are protected from the chemicals and toxic materials found in most dental offices. He has produced an environmentally friendly office that is also peaceful and calm.
He is an expert on dental materials having looked at hundreds of biocompatibility lab tests over the years. He has identified the most bio-friendly materials to use in his practice and which dental materials can be used to replace metal fillings and crowns, including BPA free and fluoride free ‘white’ fillings. He also uses metal-free Zirconia or ceramic implants and PRF (platelet-rich fibrin) grafting materials which come from the patient’s own blood.
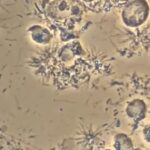
Dr. O’Rielly teaches C.E. courses on the systemic effects of gum disease. He is an expert in using phase contrast microscopy for analyzing dental infections, where he shows patients what kind of microbes, i.e. bacteria, amoeba, and yeasts like candida are populating the mouth and affecting the body as a whole.
He has an educational blog and is writing a book on dental health called ‘Hidden Dental Infections: Healing Root Canals and Infected Teeth with the Erbium Laser’ where he discusses dental nutrition, toxic dental materials and the effects of old root canals on inflammation and overall health.