I’m often asked by patients who are choosing between doing a root canal or extracting their tooth, ‘Alright doc, I get that my tooth is infected, what are my choices? What would you do if it was your tooth?’ The rest of this post discusses my best recommendations and how to choose between:
- Doing a root canal to save the tooth or
- Extracting the tooth and replacing it with a bridge or implant
This is not an easy choice as it involves treatment issues that may also have health consequences. Every day in my practice I see patients having to make this decision, so I have a lot of understanding about what’s involved and what all the considerations may be.
In the vast majority of cases, root canals are caused by infections, and the bacteria that cause root canal infections are difficult to remove completely, once they get into the tooth and the bone around the tooth.
However, extracting teeth can be very traumatic and expensive. It is a $4,000 to $5,000 proposition to extract an infected root canal and replace it with an implant and porcelain crown.
In this article, I will break down the advantages and disadvantages of each choice and give you my best advice on how to approach treatment. And there is good news as well, as you will discover.
To Extract or not to extract – An argument for saving the tooth
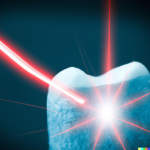
No one wants to lose a tooth. This is very natural and normal. Thanks to the advent of Photon Induced Photoacoustic streaming (PIPS), a technology licensed to Fotona utilizing the Er
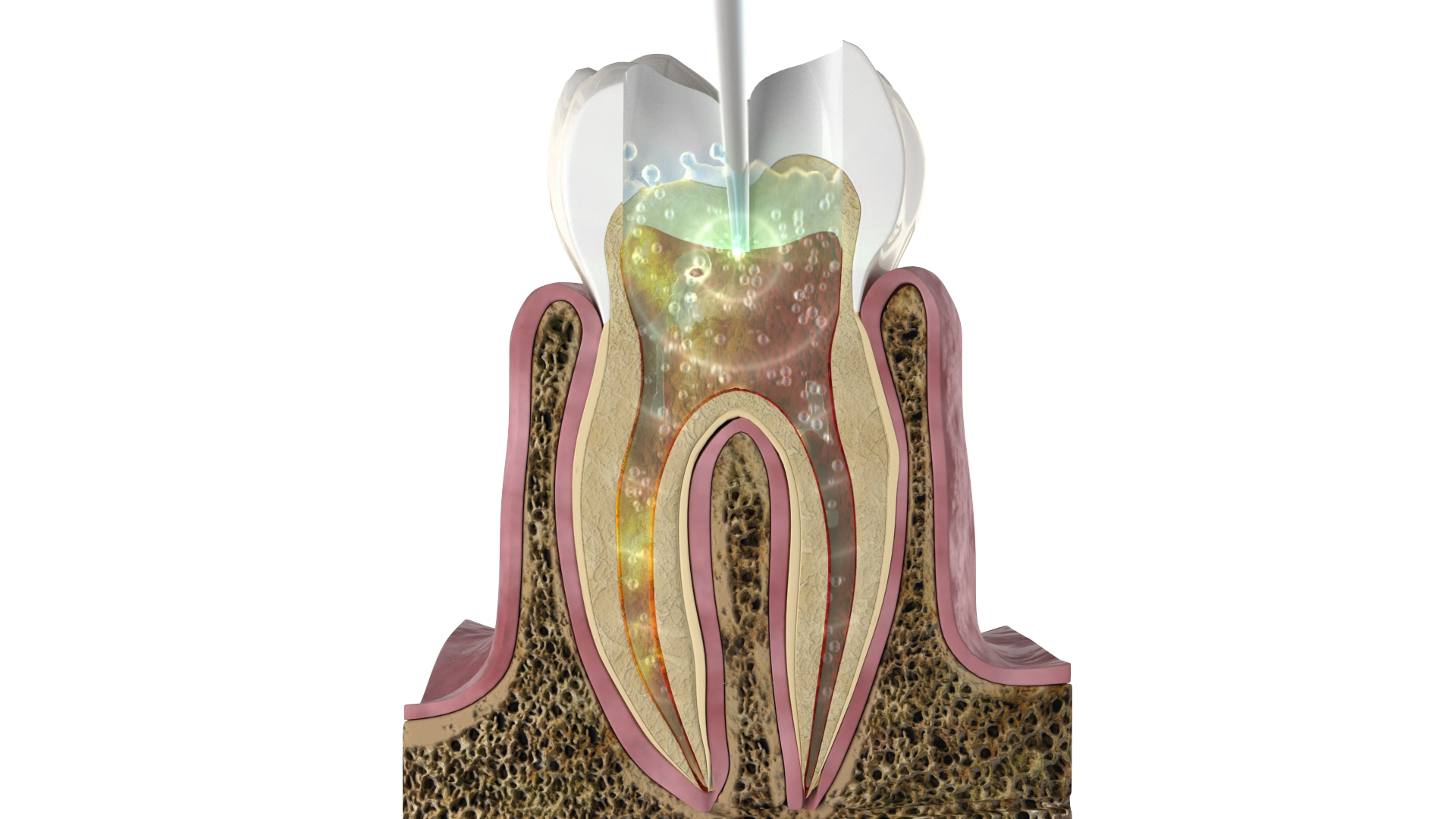
To understand the importance of this technology watch this video animation to see an example of how it works. Click on this link to see the Fotona laser in action. The reason this video is so important is that it shows what PIPS and SWEEPS can do to eliminate bacteria during root canal therapy.
I think you can clearly see what makes the PIPS technology so revolutionary. It actually reaches and kills the bacteria hiding in the dentinal tubules. Why is this important? Because the bacteria hiding in the tubules are releasing toxic material into your tooth, your jaw, and your body.
A quick review of dentinal tubules and why they are a problem
When a tooth becomes infected, it’s full of bacteria, as there are no more immune cells in the tooth. Please see my previous post discussing how this happens and showing the bacteria in the tubules of the tooth.
 To recap, the tubules are microchannels in the root connecting the inside of the tooth to the outside. They help provide the tooth with nutrients and are communication channels that allow the nerve to feel what’s happening on the surface of the tooth. They are extremely small, approximately 2 microns in diameter, but when laid side by side would be 1-2 miles long depending on the tooth.
To recap, the tubules are microchannels in the root connecting the inside of the tooth to the outside. They help provide the tooth with nutrients and are communication channels that allow the nerve to feel what’s happening on the surface of the tooth. They are extremely small, approximately 2 microns in diameter, but when laid side by side would be 1-2 miles long depending on the tooth.
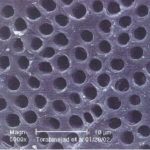
When teeth get infected the tubules get filled with bacteria and traditional root canal therapy doesn’t have an effective way of dealing with the bacteria in the tubules of the root. Below is an electron micrograph showing the tubules of a tooth.
 The problem with this bacteria is that you can’t see them on imaging or x-rays. Nor can you feel them, as they don’t cause pain. However, they are there just the same, draining endotoxins and exotoxins into your body. Endotoxins and exotoxins are fancy words for bacteria poop. Sorry to be so graphic, but this is why infected teeth are bad for you and need to be treated. It’s really the toxins caused by the bacteria that create an unhealthy situation in the tooth.
The problem with this bacteria is that you can’t see them on imaging or x-rays. Nor can you feel them, as they don’t cause pain. However, they are there just the same, draining endotoxins and exotoxins into your body. Endotoxins and exotoxins are fancy words for bacteria poop. Sorry to be so graphic, but this is why infected teeth are bad for you and need to be treated. It’s really the toxins caused by the bacteria that create an unhealthy situation in the tooth.
Why PIPS is important when doing root canals
‘So how do we get the bugs out of the tooth and tubules?’ you might ask. In his pilot study ‘Efficacy of PIPS on root canals infected with Enterococcus
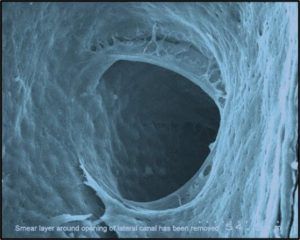 Here is an image from the study showing the tubules devoid of bacteria after treating the tooth with PIPS technology with the Fotona laser. To me as a dentist, this result is nothing short of amazing.
Here is an image from the study showing the tubules devoid of bacteria after treating the tooth with PIPS technology with the Fotona laser. To me as a dentist, this result is nothing short of amazing.
Here is another quote from a different research study. ‘All instrumentation techniques left 35% of the walls untouched.’ O. Peters, IEJ (3) 2001. In other words, when you are just using files to do root canals 35% of the tooth surface does not get cleaned because the files are not an efficient way of cleaning the canals out. In my opinion, there are bacteria left behind when using hand files and traditional root canal treatment.
In a recent advancement, Fotona has added the SWEEPS mode to do the same thing as
An argument for extracting the tooth
‘That sounds pretty good, doc. So why would you ever extract a tooth?’ you might ask. In my opinion, there are two scenarios where you would choose to extract a tooth rather than save it by doing a root canal with PIPS/SWEEPS.
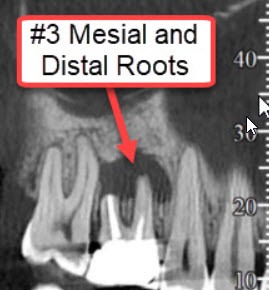 Some teeth are just too far gone. Sometimes a tooth has been worked on too many times in the past, and it is just not viable anymore. This includes too many root canals being attempted when it’s clear that there is something structurally wrong with the tooth that a root canal cannot resolve. Here is an image of an old root canal tooth that has become reinfected. See that black area at the end of the root. This is bacteria draining from the tooth even after the root canal has been done. ‘Wait a minute doc, I thought root canals were supposed to resolve tooth infections.’ Well, usually they do but not always. Additionally, the tooth can become re-infected.
Some teeth are just too far gone. Sometimes a tooth has been worked on too many times in the past, and it is just not viable anymore. This includes too many root canals being attempted when it’s clear that there is something structurally wrong with the tooth that a root canal cannot resolve. Here is an image of an old root canal tooth that has become reinfected. See that black area at the end of the root. This is bacteria draining from the tooth even after the root canal has been done. ‘Wait a minute doc, I thought root canals were supposed to resolve tooth infections.’ Well, usually they do but not always. Additionally, the tooth can become re-infected.
 Secondly, some patients are struggling with a chronic condition or disease, and it’s not a good idea to add any further possible source of inflammation. When in doubt I always recommend that my patients get the opinion of their M.D. If there are systemic factors that are not getting better, sometimes your physician may advise you to sacrifice a tooth. Inflammation is the silent killer, so the last thing you want to do is a procedure that will increase chronic inflammation. After hearing all viewpoints and opinions sometimes patients follow their intuition and decide to get the tooth out. Down the road, the tooth can still be replaced with an implant or a bridge.
Secondly, some patients are struggling with a chronic condition or disease, and it’s not a good idea to add any further possible source of inflammation. When in doubt I always recommend that my patients get the opinion of their M.D. If there are systemic factors that are not getting better, sometimes your physician may advise you to sacrifice a tooth. Inflammation is the silent killer, so the last thing you want to do is a procedure that will increase chronic inflammation. After hearing all viewpoints and opinions sometimes patients follow their intuition and decide to get the tooth out. Down the road, the tooth can still be replaced with an implant or a bridge.
‘One size does not fit all’
After reading the above, I’m sure you can see that with root canals, one approach does not fit every situation or patient. it’s impossible to generalize about what’s best for each individual. Every situation is different, including patients’ overall oral health, wants, needs, history, symptoms and the condition of the tooth itself. Many alternative doctors in the holistic and integrative health field believe that every root canal should be extracted no matter what. This, in my experience, is not accurate or realistic, as it takes a very complex issue like health and generalizes one approach for every patient and situation. Conversely, most dentists and root canal specialists recommend that the tooth try to be saved at all costs. This is also not practical or realistic in some cases, as the tooth is clearly not a good prospect for additional treatment.
I have always found that I need to approach things on a case by case basis. In order to do this, I really need to assess the situation fully and listen to what you want as a patient. How motivated are you to keep your teeth? How infected is the tooth and what are your symptoms? Are you dealing with any systemic conditions? In all cases, I try to do my best to listen to every patient’s unique needs. What do you as the patient want to do after being given all the information? In my experience, this is the only way to arrive at the right solution. It is very important that each patient make the decision that’s right for them. If I try to tell patients what I think they should do, the treatment usually does not go as well. It’s my job to give you your options, including the advantages and disadvantages of each. Then you, as the patient, can make the best decision for yourself and go forward with confidence and a full plan to resolve the infection.
What I do when I find an infected tooth or root canal
- Get
history of RCT or infected tooth, i.e. how long has it been causing a problem, is there pain and swelling, etc.? - Do thorough dental exam with x-rays and sometimes 3 D imaging
- Check bite forces, i.e. are there signs of clenching or grinding?
- How big is the infection and how long has it been there
- Is the patient suffering from any inflammatory disease
Why blood testing is important
When dealing with systemic issues like diabetes and autoimmune disease, I always recommend blood testing before any involved treatment. The reason for this is that certain inflammatory markers in the blood can signal a possible problem during the healing phase after certain dental procedures like extractions, implants and sometimes even root canals. The last thing you or I want is for there to be a failure in treatment requiring you to undo all the hard work you have put into your teeth.
There are specific markers that are designed to look at systemic inflammation including:
- Vit D levels
- Levels of immune cells
- Fibrinogen, homocysteine and especially CRP
- Blood sugar and HbA1c levels which most people don’t realize can affect your ability to heal
- Hormone levels and autoimmune markers, especially for the thyroid gland
- LDL levels and LDL/HDL ration
Dr O’s recommendations
With infected teeth and root canals, try root canal therapy first with PIPS or SWEEPS using the Fotona laser. After 34 years in practice, I finally can offer a solution that makes sense if it makes sense to the patient.
The exceptions, as discussed above, are when the tooth is broken down or fractured, the infection is just too large, or when you have a chronic condition, illness or immune issue.
Carey O’Rielly DDS has been a practicing dentist for 35 years. He went to USC Dental School and Duke University for his undergraduate degree. He grew up in Laguna Beach and now lives in La Costa with his wife Victoria, who runs his office.
He began his career by owning and operating a network of six offices in the San Francisco Bay Area. Presently he owns a private holistic practice in North County San Diego’s Encinitas.
Dr. O started looking for solutions to his health challenges that resulted from the stress and environmental toxicity that built up over a ten year period running his dental network. He has dedicated himself to learning about oral systemic problems and how dentistry can affect your health. He has applied what he has learned over the last twenty years to ensure he, his staff and his patients are protected from the chemicals and toxic materials found in most dental offices. He has produced an environmentally friendly office that is also peaceful and calm.
He is an expert on dental materials having looked at hundreds of biocompatibility lab tests over the years. He has identified the most bio-friendly materials to use in his practice and which dental materials can be used to replace metal fillings and crowns, including BPA free and fluoride free ‘white’ fillings. He also uses metal-free Zirconia or ceramic implants and PRF (platelet-rich fibrin) grafting materials which come from the patient’s own blood.
Dr. O’Rielly teaches C.E. courses on the systemic effects of gum disease. He is an expert in using phase contrast microscopy for analyzing dental infections, where he shows patients what kind of microbes, i.e. bacteria, amoeba, and yeasts like candida are populating the mouth and affecting the body as a whole.
He has an educational blog and is writing a book on dental health called ‘Hidden Dental Infections: Healing Root Canals and Infected Teeth with the Erbium Laser’ where he discusses dental nutrition, toxic dental materials and the effects of old root canals on inflammation and overall health.








Thanks for explaining that you need to consider your overall health and the condition of your tooth, among other factors, when choosing how to treat your tooth. One of my teeth has a deep cavity that will eventually need further treatment. I would like to save my tooth if possible, so a root canal would be my choice. I’ll be sure to find a good dentist that I know will do a good job.
Sometimes ozone gas can help prevent root canals when there is deep decay by oxygenating the tooth surface and killing bacteria before restoring the tooth. Good job though in saving your tooth. Did you ever find a good dentist?