As an integrative dentist, I do a lot of writing about root canals: the good, the bad and the ugly. I say ugly because I have seen a lot of bad situations with root canals over the years. Usually when root canals go bad, it’s either due to technique, materials or infection or bacteria that’s left behind. Also, infection can come back later and cause the root canal to fail. In this article I will include examples of each of these: mistakes or problems with technique, materials that cause breakdown and pathology and infection that doesn’t resolve with the root canal or that comes back later.
Teeth that are causing patients pain, problems and are draining infection into your bone and gums are failures and need to be addressed. When I say addressed I mean either retreated or extracted. It’s never a good idea to monitor or watch teeth that have any of these problems. I’m often asked what’s my position on root canals. It starts with proper diagnosis of the situation and then doing the proper treatment. My recommendations is case specific depending on the situation and the individual health signature of the patient.
The reason I’m writing this article is that I’ve seen evidence in my practice that a sizable percentage of previously done root canals are actually still infected or have become re-infected over time. Suffice it to say the percentage of undiagnosed infections due to root canals is alarmingly high. It is enough of a problem that I find myself having to speak up and start to document it with current cases.
Wait a Minute! Isn’t a Root Canal Supposed to Cure My Infected Tooth?
Yes, at least that is what you are told by your well meaning dentist. What you are not told is that the tooth you are saving by doing a root canal no longer has a blood supply or nerve. So basically you are left with a dead tooth that is cut off from the rest of your body. Blood no longer flows into your tooth so the healing components of your immune system cannot access it to heal the infection in and around it. Your tooth is cut off from your immune and lymph systems, so your body cannot fight any bacteria that’s left behind. So what happens over time is that the tooth and the bone around the tooth become re-infected with bacteria that is draining from inside the tooth, and there is nothing the body can do about it. I can’t tell you how long this problem will take because it is different for each situation and patient. However, what I can tell you is that once a root canal gets infected again, there is no way for it to heal. Antibiotics, essential oils, colloidal silver, lasers, ozone, whatever we are talking about won’t get to the source of the problem because there is no longer any blood supply to carry these things inside the tooth where the infection is.
So, Is a Root Canal a Viable Option for Me?
It depends on how much infection there is that’s present and how strong your immune system is. If you were a patient in my practice (and some of you are) this is how I would advise you:
- If there is very little bacteria and infection that has built up, this is a much better scenario for doing a root canal
- If there is infection present, you need to be careful especially if your are immune compromised, have Multiple Chemical Sensitivity (MCS) or have an auto immune condition
- If an existing root canal gets re-infected, this is where you want to seriously consider removing the tooth
Wait a minute doc. You mean take the tooth out? Unfortunately, that’s exactly what I mean. Don’t get me wrong, all dentists want to save your teeth, myself included. However, I view infections as a health concern and that is where I draw the line. For me the choice comes down to keeping a tooth or removing a chronic infection that is draining bacteria into your body 24/7. If your immune system is strong your body can deal with this for a long time. However, if your immune system is not or has been weakened over time, this may not be a good idea.
So if I Need a Root Canal or Already Have One, What Should I Do?
If you knew you had an infection in your jaw that’s draining pus from your tooth and retreating the root canal won’t fully resolve it what would you do? The most important thing is to get the right imaging. You know the typical Xrays they take in the dental office? They sometimes don’t show an infection if it’s there, even if it is a fairly large one. Why is this? It’s because the infection and pus is in your jaw, and the bone essentially masks it or hides it. The only way to be sure of what is going on is to take a 3D image of the teeth called a cone beam. This technology is becoming more available in dentistry and more dental offices and specialists are using it for their patients because of the accuracy and the information provides.
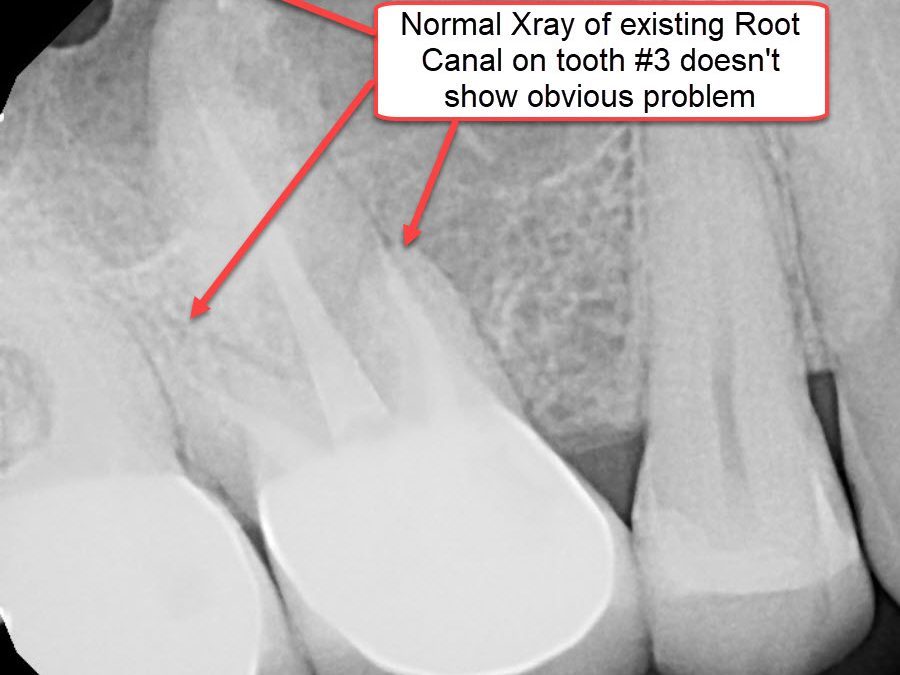
 Here is an example. In the picture to the right you see a normal dental Xray of tooth #3 which has an existing root canal. So what do you see? Well, not much. There is no clear sign of a problem. And if you combine this with the fact that this patient has no symptoms, most dentists would take a look at the tooth ask if there was any pain anywhere. If the answer was no, they pass on by and not think twice about it.
Here is an example. In the picture to the right you see a normal dental Xray of tooth #3 which has an existing root canal. So what do you see? Well, not much. There is no clear sign of a problem. And if you combine this with the fact that this patient has no symptoms, most dentists would take a look at the tooth ask if there was any pain anywhere. If the answer was no, they pass on by and not think twice about it.
Did you catch the key word in the above scenario? The key factor on whether a deeper look is done on an existing root canal tooth is if there is any pain. Pain signals there is a problem in the body and in the absence of pain everyone – including dentists – get lulled into a false sense that everything is OK. And if there is a slight sign of a problem in terms of pain or evidence on the Xray, the dentist usually puts a watch on it and doesn’t recommend treatment. The fact that there is no pain does not mean there isn’t a problem with this type of infection, as we will see below.
 Here is an image derived from a Cone Beam Xray. This is just one of dozens of images that are produced with this type of scan. See the yellow lines? Each yellow line in the image is a 1mm cross section through the tooth. As you can see, it is incredibly detailed and has the potential to reveal a lot of information about the teeth and surrounding areas. Detail that is not possible through routine Xrays.
Here is an image derived from a Cone Beam Xray. This is just one of dozens of images that are produced with this type of scan. See the yellow lines? Each yellow line in the image is a 1mm cross section through the tooth. As you can see, it is incredibly detailed and has the potential to reveal a lot of information about the teeth and surrounding areas. Detail that is not possible through routine Xrays.
This image corresponds with the root canal tooth shown in the Xray above. These images allow us to see a tooth from all angles just like we are rotating the tooth. In this way we can see if there is a problem or not. Extremely important with root canal teeth.
What Do the Cone Beam Images Show Us?
OK, let’s take slice #42 out of the image and see what it shows us.
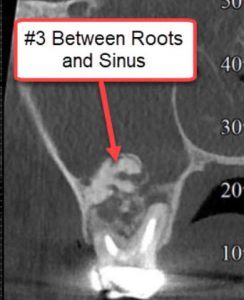 Now we get into the nitty gritty of what is going on with the root canal on tooth #3. What we see in this image is a large problem above the tooth and between the roots as pointed out by the arrow. What you are looking out here is a large infection filled with pus and granulation tissue. Granulation tissue is the body reacting to the infection.
Now we get into the nitty gritty of what is going on with the root canal on tooth #3. What we see in this image is a large problem above the tooth and between the roots as pointed out by the arrow. What you are looking out here is a large infection filled with pus and granulation tissue. Granulation tissue is the body reacting to the infection.
What you also see and what a normal Xray will never show is that the infection is going up to the sinus cavity. Sometimes old root canal teeth can actually cause a problem in the sinus cavity in terms of infection and accumulation of mucous. Again, no one would know such a problem exists unless we have the correct imaging, as you can see here.

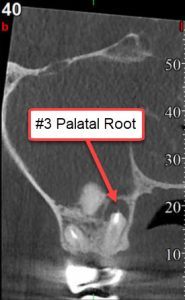 Here are two more images showing infection draining from tooth #3 into the bone. What they show are dark areas pointed out by the arrows that are essentially infection connected to the ends of the roots of the teeth. How can this happen you might ask? Remember we mentioned above that a root canal produces a dead tooth and there is no longer blood supply to the tooth? Bacteria in the tooth continues to drain out of the tooth into your bone and the body cannot keep up. You have a chronic infection that will never go away.
Here are two more images showing infection draining from tooth #3 into the bone. What they show are dark areas pointed out by the arrows that are essentially infection connected to the ends of the roots of the teeth. How can this happen you might ask? Remember we mentioned above that a root canal produces a dead tooth and there is no longer blood supply to the tooth? Bacteria in the tooth continues to drain out of the tooth into your bone and the body cannot keep up. You have a chronic infection that will never go away.
Millions of Failing Root Canals Through Reinfection
Because of the accuracy possible with 3D Cone Beam scans, I am finding that many old root canals have problems similar to what I show above. Remember that the tooth no longer has a nerve, so you don’t feel it and typically would never realize there is a problem. You and your dentist did the best you could at the time when saving your tooth seemed to be the best option and all evidence available pointed to the fact that the treatment worked. However, in light of new information provided through advanced imaging, it may be time to reconsider your options. Especially now that there are Zirconia implants available to replace teeth that are no longer viable. It’s always good to save teeth. But now that we have better technology, as shown above, it is clear that this is not necessarily the case. No pain does not mean success.
The American Association of Endodontists estimates that 18 million root canals are done in this country per year. That is a lot of root canals. What happens when those root canals start to fail and get infected again? This is why I’m writing this book, ‘The Tooth Body Connection: The Coming Cycle of Failing Root Canals in America.’ I feel this is going to be a mounting and ongoing problem in dentistry today and into the future. Once we can see the problem produced by our prior treatment, dentists in this country are going to be surprised and caught off guard. There is no way they could have known what they were causing at the time in their attempts to save teeth. Now the problem is going to be exposed for everyone to see through Cone Beam (3D) technology.
If you have an experience regarding root canals that you would like to share so that others can benefit, please feel free to comment below. Also, if you have a question feel free to put in the comment section and I will personally respond to you by email.
Thanks for reading. If you would like to have me evaluate your root canal teeth or if you are not sure you need one, you may come visit me in my practice and we can discuss it. My contact information is below.
Dr. Carey ORielly
Carey O’Rielly DDS has been a practicing dentist for 35 years. He went to USC Dental School and Duke University for his undergraduate degree. He grew up in Laguna Beach and now lives in La Costa with his wife Victoria, who runs his office.
He began his career by owning and operating a network of six offices in the San Francisco Bay Area. Presently he owns a private holistic practice in North County San Diego’s Encinitas.
Dr. O started looking for solutions to his health challenges that resulted from the stress and environmental toxicity that built up over a ten year period running his dental network. He has dedicated himself to learning about oral systemic problems and how dentistry can affect your health. He has applied what he has learned over the last twenty years to ensure he, his staff and his patients are protected from the chemicals and toxic materials found in most dental offices. He has produced an environmentally friendly office that is also peaceful and calm.
He is an expert on dental materials having looked at hundreds of biocompatibility lab tests over the years. He has identified the most bio-friendly materials to use in his practice and which dental materials can be used to replace metal fillings and crowns, including BPA free and fluoride free ‘white’ fillings. He also uses metal-free Zirconia or ceramic implants and PRF (platelet-rich fibrin) grafting materials which come from the patient’s own blood.
Dr. O’Rielly teaches C.E. courses on the systemic effects of gum disease. He is an expert in using phase contrast microscopy for analyzing dental infections, where he shows patients what kind of microbes, i.e. bacteria, amoeba, and yeasts like candida are populating the mouth and affecting the body as a whole.
He has an educational blog and is writing a book on dental health called ‘Hidden Dental Infections: Healing Root Canals and Infected Teeth with the Erbium Laser’ where he discusses dental nutrition, toxic dental materials and the effects of old root canals on inflammation and overall health.







I started having ear pain but we couldn’t figure out which 2 teeth on the lower back left molars was hurting. So I waited hoping to figure out the right tooth. Waited too long. Now my Endodontist did the molar in front of the back with a root canal. Then I got a 2nd opinion to do a retreat on the back molar next to it with a previous root canal. Still having ear pain and problems. Dr checked my surrounding teeth trying to find the problem and did a root canal on my upper back molar thinking the big mercury filing was the problem. I have Hashimoto and think I will have the back molar just pulled. You can see the abcess and hole in jaw in the X-ray. Still have ear pain and tooth throbbing off and on. The tooth with the 1st root canal of the inside molar hurts to touch it and floss. We can’t figure that out. Dr wants to retreat it. I counted and I now have 8 root canals. ☹️Should I find a new endodontist? Costing a fortune. Good Dr’s 32 years experience but can’t figure this mess out. I think the problem is the inside molar we did the 1st root canal on. It shouldn’t hurt to touch it or floss. I don’t think according to what you’ve said the retreating it will help for very long. Worried about my health and all this infection. Thank you for your help.. ❤️
does extracting the infected failed rc tooth and antibiotics clear up the infection? The blood supply should return to the area once extracted, correct ?
I had a root canal on tooth number 30 about 2 years ago. For a year there was no problem. Then that area of the tooth started getting very tender and hurt when a chewed. I kept letting it go hoping it would just go away but it didn’t. I went back to that dentist and he said the tooth was infected. He prescribed an anti-biotic and told me if that didn’t work, he’d have to go back into the tooth. The pain has spread to around my right neck area and right side jaw. Now, the pain at the actual tooth has lessened a lot but the pain around my right neck and like area around the back of my right ear has not gone away. I have an appointment to go back on Feb. 6 for him to go back into the tooth.
What do you think the success rate would be? The actual tooth is part of a 29-30-31 unit bridge. I’ve been dealing with this at least a year. Is it common to feel muscular pain around the neck area in the area of the tooth? Oh, also i’m hearing this crunching sound in my right ear when I open and close my mouth.
I guess at this point, I’ll go thru with him going back into the tooth. Are we fighting a loss cause? Would it be better to go to an endodontist although that would probably be more expensive than going back to the dentist that did this work. I live in the St. Louis, MO area.
Dear Richard, that certainly does not sound good for that tooth. It sounds infected. If you end up extracting the tooth then a bridge is an option for sure. Good luck!
How can I get a dentist here in clovis/fresno, ca check for infection from a root canal. What tests should I ask for. Doesn’t seem that anyone here in even has the technology to check for infrection. I have ear aches, sinus problems, twitching in my left eye, pain every day and night. What do I do? I asked dentist to pull the teeth but he didn’t listen to me.
Try the IAOMT. If you need to look deeper for possible infections around root canal teeth, you will need to take a Cone Beam X-ray.
I just watched “root cause” which just opened my eyes I have had declining health issues for some time.brain fog, achy joints,low back pain, tired even though I’ve had a full nights sleep and burning in my esophagus.a suppressed immune system. My physicals blood tests repeatedly show infection and inflammation in my body. I have 5 root Canals and I’m not sure how to remove these root canals and still look normal and eat normal. What can someone like me do? I about to have a cone beam scan to see any signs of infection but then what if I do ?or what if I don’t? Do you remove only the one’s that are infected? Any advice would be greatly appreciated. Nicole
Hi Nicole, Did you ever take that Cone Beam, and if you did what did it show? If any of those root canal teeth are infected, they should definitely be treated.