Last weekend I gave a lecture in San Diego about how bacteria in the mouth can infect the rest of our bodies and have been linked to diseases like heart disease and Alzheimer’s. If you have bleeding gums when you brush or floss or if you have root canals, you are going to want to read more of what I’m going to go over in my next posts.
 Can the microbiome in your mouth affect the microbiome in your gut? The answer is yes, according to a study in the Journal of Oral Microbiology, published in March of 2019. More on this later. First, let’s explore what the microbiome is and why it’s so important. We are actually walking, talking microbial ecosystems.
Can the microbiome in your mouth affect the microbiome in your gut? The answer is yes, according to a study in the Journal of Oral Microbiology, published in March of 2019. More on this later. First, let’s explore what the microbiome is and why it’s so important. We are actually walking, talking microbial ecosystems.
The microbiome is the community of trillions of bacteria and other organisms living in and on us. The majority of those invisible organisms are in our intestinal tract. A balanced ecology of the different microbes that reside in the gut is really important because 70% of our immune cells line the gut.
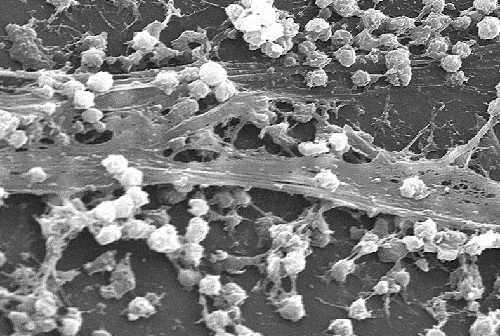
The microbiome in the mouth can become imbalanced through some different factors, including the way that bacteria congregate in the mouth. This has to do with what’s known as biofilm. Biofilm is the sticky residue that adheres around your gum line. The sticky residue is commonly known as plaque. It actually consists of bacterial colonies that stick to each other and to a particular surface. In the case of the mouth, it sticks to your teeth along the gum line and in between them.
That’s why in our practice we give out what we call a ‘rubber tip’. Here’s how it looks.
 Its actual name is a Stimulator made by GUM. If you’re aren’t one of my patients, you can get one online. How you use it is, you wipe the tooth along the scalloped edges of your gum line. You are rubbing the plaque off your tooth surface along the gums and not pressing into your gums. You wipe off any of the sticky white stuff that might come off. You won’t always see that happening, but it’s enough to disrupt the hidden biofilm that’s sticking to your teeth. You’ll want to use the rubber tip on all your teeth, front, back, top and bottom once a day. This is a simple and effective way to keep your mouth healthy.
Its actual name is a Stimulator made by GUM. If you’re aren’t one of my patients, you can get one online. How you use it is, you wipe the tooth along the scalloped edges of your gum line. You are rubbing the plaque off your tooth surface along the gums and not pressing into your gums. You wipe off any of the sticky white stuff that might come off. You won’t always see that happening, but it’s enough to disrupt the hidden biofilm that’s sticking to your teeth. You’ll want to use the rubber tip on all your teeth, front, back, top and bottom once a day. This is a simple and effective way to keep your mouth healthy.
Why is the microbiome suddenly a hot topic? Up until the last 10-15 years scientists were only able to study human microbes by growing them in the lab. However, this approach won’t work with most of the microbes in the body, so that area of research has been very limited. As better technology has become available, it’s currently possible to actually study the DNA of these microbes!
Research has now found that there are over 1000 different types of bacteria living in the human body, microbes that are important for your gut, heart, brain and other organs. There are 40 trillion bacterial cells the body, so many that they actually outnumber our own 30 trillion human cells! Additionally there are fungi, viruses and other microbes.
The title of the study I referred to earlier in this post, published last year is: ‘Can oral bacteria affect the microbiome of the gut?’
J Oral Microbiol. 2019; 11(1): 1586422.
Published online March 2019 doi:
Here are some of the findings of the study, published by the National Center for Biotechnology Information, a division of the U.S. National Institute of Health:
Oral bacteria circulating in the body have been linked with a number of systemic diseases, including diseases of the gut. But how do these microbes get into the different parts of the digestive tract? There are three ways:
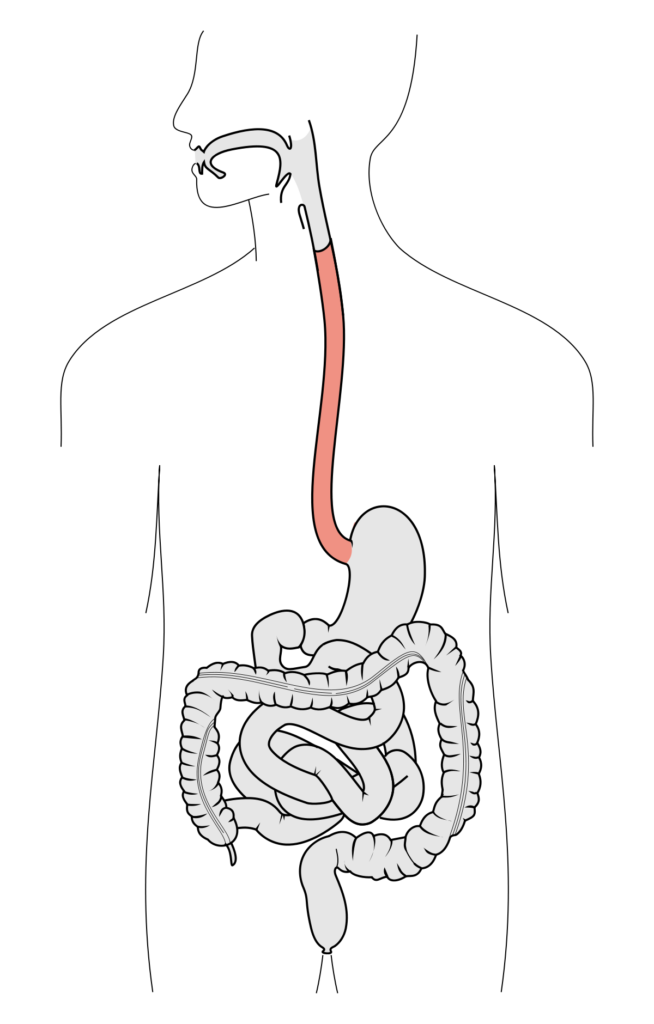 1) Microbes from the mouth directly penetrate the esophagus, which is the muscular tube that connects the throat with the stomach. This can be enough to unbalance the ecosystem of the digestive tract.
1) Microbes from the mouth directly penetrate the esophagus, which is the muscular tube that connects the throat with the stomach. This can be enough to unbalance the ecosystem of the digestive tract.
2) Bleeding gums that occur because of gingivitis and gum disease, can give oral microbes access to the bloodstream. This allows these microorganisms to circulate systemically.
3) There have been recent advances in identifying microbial metabolites that directly affect the gastrointestinal tract. Metabolites is a fancy word for bacteria poop and other by-product of microbial metabolism. These metabolites can lead to various chronic diseases of the digestive tract and they are also absorbed into the blood steam, causing a low grade inflammatory state.
Oral bacteria and other microbes found in the mouth can reach the stomach through swallowed saliva, nutrients, and drinks. These bacteria generally don’t colonize in a healthy intestine, but in certain cases, particularly when there is gum disease, they will multiply. This sets off the intestinal immune system, causing chronic inflammation.
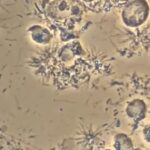
One of the three worst offenders identified as causing gum disease (periodontal disease) is P. gingivalis. In the image below the black circles are P. gingivalis. It is now being found in the gut, where it can cause dysregulaton.
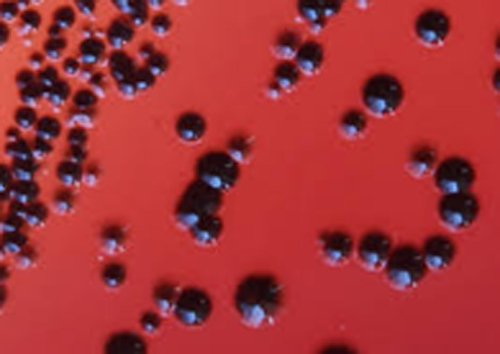 Gut dysregulation or dysbiosis is another way of saying ‘leaky gut’. This happens when the tight junctures keeping the gut intact start to ‘leak’, allowing food particles and toxins to pass back into the bloodstream. This can cause inflammation and sometimes a response from the immune system. What this study is suggesting that P. Gingivalis is able to find its way to the gut, causing dysbiosis and possibly disease.
Gut dysregulation or dysbiosis is another way of saying ‘leaky gut’. This happens when the tight junctures keeping the gut intact start to ‘leak’, allowing food particles and toxins to pass back into the bloodstream. This can cause inflammation and sometimes a response from the immune system. What this study is suggesting that P. Gingivalis is able to find its way to the gut, causing dysbiosis and possibly disease.
That’s why if you have inflamed gums that bleed when you brush or floss, or if your teeth are loose or move, be sure to get this checked out on your next hygiene visit. These are all indicators of gingivitis, which, as you’ve now learned, can have consequences for your systemic health.
There are also plenty of ‘good microbes’ in the gut that you’ll want to encourage with good habits and a good diet. Probiotics are another way to help beneficial bugs to thrive, especially when there has been antibiotic use.
We have known for a while now that there were direct links between the bacteria and microbiome of the mouth and systemic diseases, but now we are starting to prove what the actual offenders are, like P. gingivalis. Once we can identify the actual offenders we can start to design treatments to address these infections and improve our health.
In my next posts I’ll discuss more DIY tips and tricks that you can use at home to keep your oral microbiome balanced and healthy. As we’ll see, this will protect not only your gut and gums, but also your heart and brain. For example the most researched bacteria associated with root canal infections, Enterococcus faecalis, has been found in the heart. Stay tuned for this extremely important connection between root canals and heart health and what you can do about it.
Thanks for reading this post and taking the time to learn more about oral systemic health.
Carey O’Rielly DDS has been a practicing dentist for 35 years. He went to USC Dental School and Duke University for his undergraduate degree. He grew up in Laguna Beach and now lives in La Costa with his wife Victoria, who runs his office.
He began his career by owning and operating a network of six offices in the San Francisco Bay Area. Presently he owns a private holistic practice in North County San Diego’s Encinitas.
Dr. O started looking for solutions to his health challenges that resulted from the stress and environmental toxicity that built up over a ten year period running his dental network. He has dedicated himself to learning about oral systemic problems and how dentistry can affect your health. He has applied what he has learned over the last twenty years to ensure he, his staff and his patients are protected from the chemicals and toxic materials found in most dental offices. He has produced an environmentally friendly office that is also peaceful and calm.
He is an expert on dental materials having looked at hundreds of biocompatibility lab tests over the years. He has identified the most bio-friendly materials to use in his practice and which dental materials can be used to replace metal fillings and crowns, including BPA free and fluoride free ‘white’ fillings. He also uses metal-free Zirconia or ceramic implants and PRF (platelet-rich fibrin) grafting materials which come from the patient’s own blood.
Dr. O’Rielly teaches C.E. courses on the systemic effects of gum disease. He is an expert in using phase contrast microscopy for analyzing dental infections, where he shows patients what kind of microbes, i.e. bacteria, amoeba, and yeasts like candida are populating the mouth and affecting the body as a whole.
He has an educational blog and is writing a book on dental health called ‘Hidden Dental Infections: Healing Root Canals and Infected Teeth with the Erbium Laser’ where he discusses dental nutrition, toxic dental materials and the effects of old root canals on inflammation and overall health.