Whenever I go to an implant meeting these days a lot of what’s being discussed is titanium implant failures and what to do about them. I went to two high level conventions in 2016 and I was surprised at all the case studies presented highlighting failures of titanium implants. Much of the focus was on maintaining these implants in the face of significant inflammation and progressive bone loss. This condition is called peri-implantitis and is similar to periodontal disease or gum disease. The difference is that peri-implantitis is gum disease that happens around implants. Periodontal disease is gum disease that happens around natural teeth. Basically, both result in loss of bone and gum support due to infection from bacteria and the inflammation that results. Eventually the infection starts to drain pus from around the affected tooth or implant resulting in pain, soreness and possibly the loss of the implant altogether. The above graphic is of the annual convention of implantologists, oral surgeons and dentists attending high level lectures on implant techniques.
 The graphic on the right was another meeting of periodontists/gum specialists discussing gum procedures and implants. Fully 1/4 to 1/3rd of the lectures had to do with how to manage and try to fix failing implants and what to do with the growing problem of peri-implantitis.
The graphic on the right was another meeting of periodontists/gum specialists discussing gum procedures and implants. Fully 1/4 to 1/3rd of the lectures had to do with how to manage and try to fix failing implants and what to do with the growing problem of peri-implantitis.
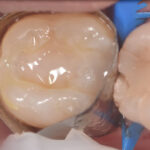
Basically, the case studies presented discussed what treatment options there are to keep the implants in place for as long as possible by slowing down the disease process. At this point there is quite a bit of agreement that once the core of the implant is exposed to the oral cavity bacteria can then start to attach or imbed itself onto the surface of the implant because it is rough. It can also create deposits in the grooves of the implant similar to the build up and plaque on your teeth that your dentist removes every 6 months during your cleaning appointment. The problem is that these deposits on implants result in bone loss with implants much, much faster than with natural teeth, because the strength of the gum and bone attachments to the implant is much weaker than with real teeth.
The recommended treatment is to pull the gum back from the implant so that it can be smoothed and polished as best as possible. This makes it harder for bacteria to continue to attach to the implant and infect the bone around it. This definitely slows down the damage from peri-implantitis, but by that time the metal from the implant usually starts to show as a black band or as a gray halo through the gums. This is a failure by most dentists criteria and cosmetically it is certainly a failure for the patient.
2016 began a sea change in how titanium implants are going to be viewed by the profession and by the public at large. Peri-implantitis is a huge problem because there is no real fix and the number of cases are just going to grow as time goes on as more and more implants are being placed every year. I’ve even heard the word epidemic be thrown out by some practitioners and lecturing implant experts.
So what’s the solution? In my next post I’ll review the causes of peri-implantitis and what to do to avoid them. Hint: stop doing the procedure that causes it.
Carey O’Rielly DDS has been a practicing dentist for 35 years. He went to USC Dental School and Duke University for his undergraduate degree. He grew up in Laguna Beach and now lives in La Costa with his wife Victoria, who runs his office.
He began his career by owning and operating a network of six offices in the San Francisco Bay Area. Presently he owns a private holistic practice in North County San Diego’s Encinitas.
Dr. O started looking for solutions to his health challenges that resulted from the stress and environmental toxicity that built up over a ten year period running his dental network. He has dedicated himself to learning about oral systemic problems and how dentistry can affect your health. He has applied what he has learned over the last twenty years to ensure he, his staff and his patients are protected from the chemicals and toxic materials found in most dental offices. He has produced an environmentally friendly office that is also peaceful and calm.
He is an expert on dental materials having looked at hundreds of biocompatibility lab tests over the years. He has identified the most bio-friendly materials to use in his practice and which dental materials can be used to replace metal fillings and crowns, including BPA free and fluoride free ‘white’ fillings. He also uses metal-free Zirconia or ceramic implants and PRF (platelet-rich fibrin) grafting materials which come from the patient’s own blood.
Dr. O’Rielly teaches C.E. courses on the systemic effects of gum disease. He is an expert in using phase contrast microscopy for analyzing dental infections, where he shows patients what kind of microbes, i.e. bacteria, amoeba, and yeasts like candida are populating the mouth and affecting the body as a whole.
He has an educational blog and is writing a book on dental health called ‘Hidden Dental Infections: Healing Root Canals and Infected Teeth with the Erbium Laser’ where he discusses dental nutrition, toxic dental materials and the effects of old root canals on inflammation and overall health.